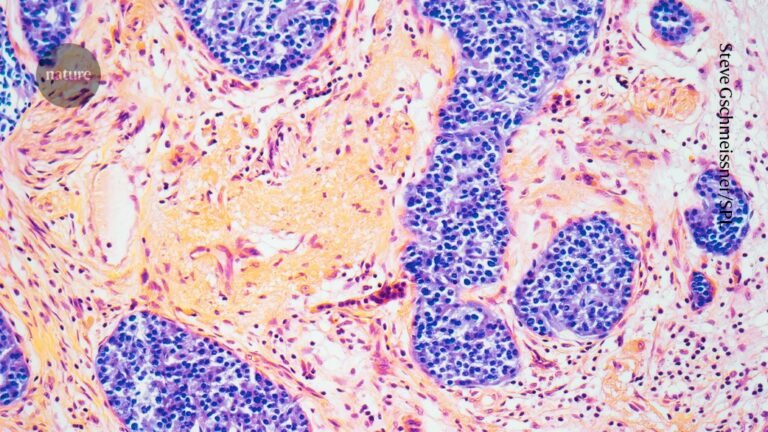
The condition called pancreatitis causes inflammation of the pancreatic tissue (pictured). Credit: Steve Gschmeissner/Science Photo Library
The potent GLP-1 drugs are taken by millions of people worldwide to counter obesity, heart disease, diabetes and more. However, a rare and potentially fatal illness that might be linked to these blockbuster therapies is now causing alarm in some countries.
Last month, the United Kingdom issued a warning about the possible link between drugs that mimic a hormone called glucagon-like peptide-1 (GLP-1) and acute pancreatitis, an inflammation of the pancreas. Since 2007, the country has recorded 19 deaths from pancreatitis in people taking GLP-1 drugs. Brazil, which has registered six deaths in the past five years, issued its own warning ten days later.
The risk of pancreatitis is already listed in information leaflets provided to people taking the drugs. But a large increase in the number of pancreatitis reports in recent years, including severe cases and deaths, prompted the UK Medicines and Healthcare products Regulatory Agency (MHRA) to strengthen its warning, says Alison Cave, chief safety officer at the MHRA.
But it’s not clear whether the drugs actually cause the disease, says Jaime Almandoz, an endocrinologist and obesity specialist at the University of Texas Southwestern Medical Center in Dallas. As the use of GLP-1 drugs increases, reports of side effects are likely to become more common, he says. Vigilant monitoring and rigorous studies are needed “to help refine our understanding of these rare adverse events”.
Here’s what the evidence suggests about this potential risk.
What do we know about the deaths?
The 19 deaths recorded in the United Kingdom were reported between 2007 and October 2025. In the same period, nearly 1,300 reports of pancreatitis associated with GLP-1 drugs were reported to health officials. The six deaths in Brazil were reported from 2020 to December 2025, as were 145 cases of pancreatitis in people taking GLP-1 medications. Widespread use of the drugs to treat obesity began in 2021.
Anti-obesity drugs’ side effects: what we know so far
Considering the number of people taking these drugs — in Great Britain alone, an estimated 1.6 million adults used GLP-1 medications between early 2024 and early 2025 — the risk of developing these side effects is very small, says Cave. By comparison, thousands of people are hospitalized with pancreatitis in Britain every year.
Cave adds that it’s very challenging to determine whether the cases of pancreatitis were directly caused by the drugs because many people on these medications already have an increased risk for pancreatitis to begin with.
Furthermore, anyone can report drug side effects to the UK and Brazilian databases that were the source of the case numbers. As a result, “it’s hard to sort out the noise from the real signal”, says Beverly Tchang, an endocrinologist at Weill Cornell Medicine in New York City.
What do clinical trials show?
“Data about the risk of pancreatitis with GLP-1 use has been very heterogeneous,” says Ebubekir Daglilar, a gastroenterologist at West Virginia University in Charleston.
A 2025 meta-analysis1 of 62 randomized controlled clinical trials of several GLP-1 drugs found that that people on these medications had a slightly increased risk of pancreatitis compared with those on a placebo. But other analyses2,3 found no such association.
In an effort to provide an answer to patients who were hesitant about taking the drugs because of possible side effects, Daglilar and his colleagues decided to analyse information from a large medical data set. They compared the risk of pancreatitis between two groups, each comprising nearly 82,000 people with type 2 diabetes. The groups had similar risk factors for pancreatitis, but people in one group were taking GLP-1 drugs and people in the other group were not. The researchers found no difference in pancreatitis rates between the two4.